Is Arthritis Hereditary?
What is Arthritis?

Arthritis is a common but often misunderstood condition that affects millions of people worldwide. It is not a single disease but a term encompassing a group of more than 100 types of joint disorders.
These conditions can cause pain, swelling, stiffness, and decreased joint mobility, significantly impacting the quality of life for those affected.
In this blog post, we will delve into the various aspects of arthritis, exploring its types, causes, and symptoms, and will learn: Is Arthritis Hereditary?
Types of Arthritis:
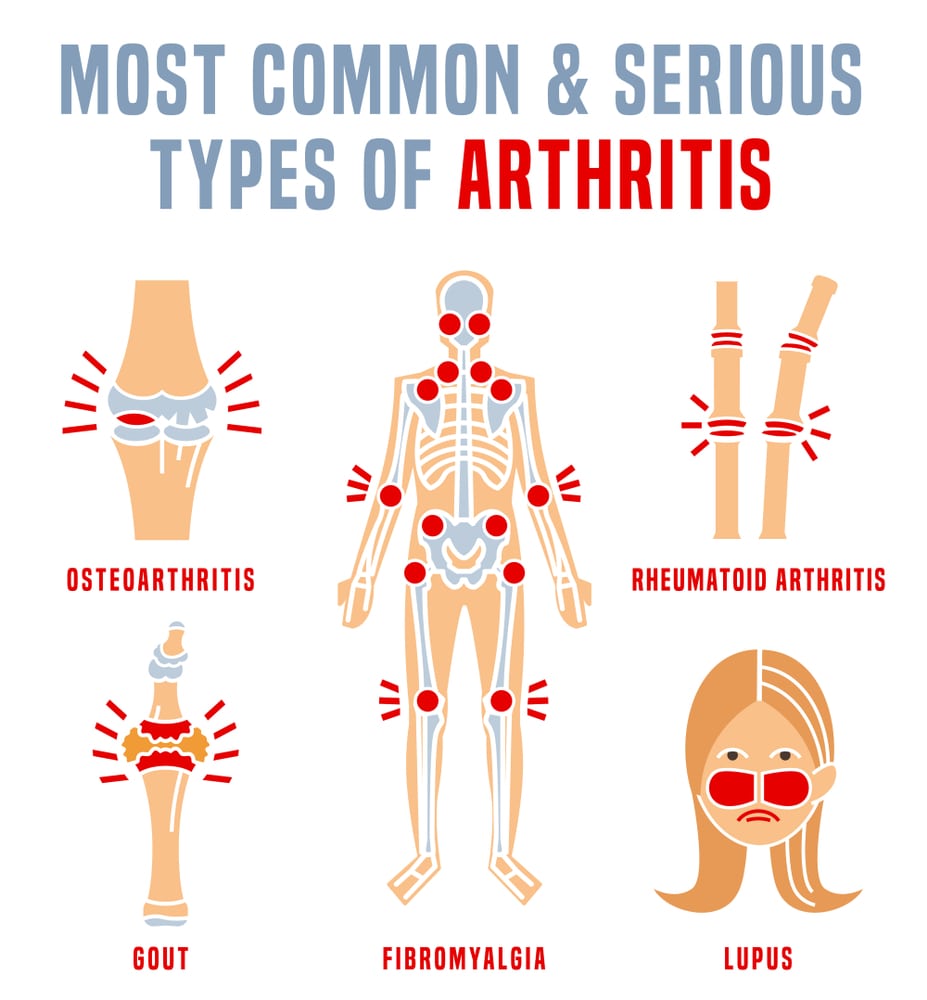
- Osteoarthritis (OA): This is the most prevalent form of arthritis, often referred to as “wear and tear” arthritis. It occurs when the protective cartilage cushions the ends of bones and wears down over time.
- Rheumatoid Arthritis (RA): An autoimmune disorder where the immune system attacks the joints, causing inflammation. It can affect not only joints but also organs.
- Psoriatic Arthritis: Associated with the skin condition psoriasis, this type of arthritis affects both the skin and joints.
- Ankylosing Spondylitis: Primarily affects the spine, causing inflammation and stiffness.
- Gout: Caused by the accumulation of uric acid crystals in the joints, leading to inflammation.
What causes Arthritis?

- Age: Osteoarthritis, the most common form of arthritis, is often associated with aging. As people get older, the wear and tear on joints accumulate, leading to the breakdown of cartilage.
- Genetics: Is Arthritis Hereditary? Yes. Some forms of arthritis, such as rheumatoid arthritis and ankylosing spondylitis, have a genetic component. Individuals with a family history of arthritis may be at a higher risk.
- Autoimmune Factors: In autoimmune arthritis, such as rheumatoid arthritis, the immune system mistakenly attacks the synovium (the lining of the membranes surrounding the joints), leading to inflammation and joint damage. The exact cause of this autoimmune response is not fully understood, but it likely involves a combination of genetic and environmental factors.
- Infections: Infections can trigger certain types of arthritis. For example, bacterial or viral infections can lead to reactive arthritis, where the body’s immune system responds to the infection by attacking the joints.
- Joint Injury: Trauma or injury to a joint, such as a fracture or dislocation, can increase the risk of developing arthritis in that joint. Post-traumatic arthritis may develop years after an injury.
- Metabolic Abnormalities: Conditions that affect metabolism, such as gout, can lead to arthritis. Gout is caused by the build-up of uric acid crystals in the joints, resulting in inflammation and pain.
- Obesity: Excess body weight puts additional stress on the joints, particularly in the knees, hips, and spine. This can contribute to the development or progression of arthritis, especially osteoarthritis.
- Hormonal Factors: Hormonal changes, particularly in women, may contribute to the development of certain types of arthritis. For example, rheumatoid arthritis is more common in women, and its onset is often associated with hormonal changes.
How to Diagnose Arthritis?

Here is a general overview of the diagnostic process for arthritis:
- Medical History: The doctor will begin by taking a detailed medical history. This includes asking about the nature and duration of symptoms, any family history of arthritis, past injuries or surgeries, and overall health.
- Physical Examination: A thorough physical examination assesses joint function, swelling, tenderness, and range of motion. The doctor may also check for signs of inflammation, such as warmth and redness around the joints.
- Laboratory Tests: Blood tests are often used to help diagnose arthritis and differentiate between different types. Standard blood tests include Rheumatoid Factor (RF), Anti-cyclic citrullinated peptide (anti-CCP) antibodies, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), Complete Blood Count (CBC).
- Imaging Studies: X-rays, magnetic resonance imaging (MRI), and computed tomography (CT) scans can provide detailed images of the joints and surrounding structures. These imaging studies help identify joint damage, narrowing of joint spaces, and other abnormalities. X-rays are particularly useful for diagnosing osteoarthritis, while MRI and CT scans are more sensitive in detecting soft tissue and early joint changes.
- Joint Aspiration (Arthrocentesis): In this procedure, a small amount of fluid is withdrawn from the affected joint using a needle. The fluid is then analyzed for signs of infection, crystals (as seen in gout), and inflammation.
How to treat Arthritis?

The treatment of arthritis aims to manage symptoms, reduce inflammation, improve joint function, and enhance overall quality of life.
Here are common strategies used in the treatment of arthritis:
1. Medications:
- Pain Relievers (Analgesics): Over-the-counter pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) can help manage pain. Example: Ibuprofen, Diclofenac, and Acelcofenac.
- Disease-Modifying Anti-Rheumatic Drugs (DMARDs): These medications, such as methotrexate, are often used in autoimmune arthritis like rheumatoid arthritis to slow disease progression and preserve joint function. Example: Methotrexate, Hydroxychloroquine.
- Biologics: These drugs, such as tumor necrosis factor (TNF) inhibitors, target specific components of the immune system to reduce inflammation in autoimmune arthritis. Example: Adalimumab and Certolizumab.
- Corticosteroids: Injections or oral medications may be prescribed for short-term relief of severe inflammation. Examples: Cortisone and Prednisolone.
2. Lifestyle Modifications:
- Exercise: Regular physical activity helps maintain joint flexibility, strengthen muscles around the joints, and reduce pain. Low-impact activities such as swimming and walking are often recommended.
- Weight Management: Maintaining a healthy weight reduces stress on weight-bearing joints, such as the knees and hips, and can alleviate symptoms of arthritis.
- Joint Protection: Techniques such as using assistive devices, wearing supportive shoes, and avoiding excessive repetitive motions can protect joints from further damage.
3. Physical Therapy:
A physical therapist can design an exercise program tailored to an individual’s needs, focusing on improving joint function, flexibility, and strength.
4. Occupational Therapy:
Occupational therapists can provide strategies and tools to help individuals manage daily activities with reduced joint strain.
5. Assistive Devices:
Devices such as braces, splints, and canes can support and reduce stress on affected joints.
6. Surgery:
In severe cases where joint damage is extensive, surgical options may be considered. Joint replacement surgery, such as hip or knee replacement, can significantly improve mobility and reduce pain.
7. Alternative Therapies:
- Acupuncture: Some people find relief from arthritis symptoms through acupuncture, an alternative therapy that involves the insertion of thin needles into specific points of the body.
- Massage: Massage therapy may help relax muscles, improve circulation, and reduce pain and stiffness.
Is Arthritis Hereditary?

Yes, Arthritis is hereditary. Arthritis, a term encompassing over 100 different types of joint disorders, affects millions of people worldwide. One common question that often arises is whether arthritis has a hereditary component.
The Genetic Landscape of Arthritis:
- Rheumatoid Arthritis (RA): RA has a clear genetic link. Specific genes, such as HLA-DRB1, have been identified as risk factors for developing rheumatoid arthritis. However, having these genes doesn’t guarantee the development of RA, and environmental factors also play a significant role.
- Osteoarthritis (OA): While OA is often thought of as a consequence of aging and joint wear and tear, there is evidence of a genetic component. Individuals with a family history of osteoarthritis may be more predisposed to developing the condition.
- Ankylosing Spondylitis (AS): Ankylosing spondylitis has a strong genetic association, with the HLA-B27 gene being a key marker. However, not everyone with this gene develops AS, highlighting the influence of other factors.
- Psoriatic Arthritis: Psoriatic arthritis is more common in individuals with a family history of psoriasis. Genetic markers, including HLA-B27, contribute to the hereditary aspect of this form of arthritis.
- Gout: Gout has a hereditary component, with some families having a genetic predisposition to elevated uric acid levels. However, lifestyle factors, such as diet and alcohol consumption, also play a crucial role in gout development.
Understanding the Complexity: Is Arthritis Hereditary?
While there is a genetic predisposition to certain types of arthritis, it’s crucial to understand that genetics alone do not determine the fate of an individual’s joint health. The interplay of environmental factors, lifestyle choices, and genetic predispositions creates a complex landscape.
- Environmental Factors: Exposure to certain environmental triggers, such as infections or toxins, can influence the development of arthritis. These factors interact with genetic susceptibility to contribute to the onset of the condition
- Lifestyle Choices: Lifestyle factors, including diet, exercise, and weight management, play pivotal roles in arthritis development. Maintaining a healthy lifestyle can mitigate the impact of genetic predisposition.
Endnote:
In the quest to understand arthritis and the question: Is Arthritis hereditary, it becomes evident that genetics is just one piece of the puzzle. Arthritis is a multifaceted condition influenced by a combination of genetic, environmental, and lifestyle factors.
By gaining insights into one’s genetic predisposition and adopting a proactive and informed approach to joint health, individuals can navigate the complexities of arthritis, ultimately enhancing their overall well-being.
FAQs
Is gout arthritis?
Yes, it is a complex form of arthritis.
Are tomatoes bad for arthritis?
Yes, researchers have been supportive of the fact that tomatoes are bad for arthritis and joint pains.
Does arthritis cause swelling?
Yes, arthritis causes joints to swell.
Does cracking your knuckles cause arthritis?
No, this is quite not true.
Is arthritis a disability?
You may be eligible for disability if your inflammatory arthritis affects your axial spine (such as psoriatic arthritis) or your peripheral joints (such as Rheumatoid arthritis, Psoriatic arthritis, etc.). It can raise the question: Is arthritis hereditary? Yes, some of the diseases are hereditary and can turn into disability.
References:
- https://www.mayoclinic.org/diseases-conditions/arthritis/symptoms-causes/syc-20350772
- https://www.arthritis.org/health-wellness/about-arthritis/understanding-arthritis/what-is-arthritis
- https://www.voltarengel.com/living-with-arthritis/is-arthritis-hereditary/
- https://health.clevelandclinic.org/is-arthritis-hereditary/

