How To Prevent Gestational Diabetes?
Gestational diabetes is a temporary type of diabetes that develops during pregnancy and affects around 2-10% of pregnant women. It occurs when the body cannot produce enough insulin to regulate blood sugar levels adequately. Although it usually goes away after childbirth, gestational diabetes can have serious implications for both the mother and the baby if not managed properly.
The good news is that it’s often preventable with a few lifestyle changes and regular monitoring. In this blog, we’ll explore practical steps on how to prevent gestational diabetes and ensure a healthy pregnancy.
What is Gestational Diabetes?

Women who did not have diabetes before getting pregnant can develop gestational diabetes, a form of the disease, during pregnancy. It is a temporary condition that typically develops in the second or third trimester when the body is unable to produce enough insulin to meet the increased demands of pregnancy.
Gestational Diabetes is different from other types of diabetes, such as type 1 or type 2 diabetes. The condition of gestational diabetes is typically diagnosed through routine prenatal screenings. Many women with gestational diabetes do not show any noticeable symptoms, which is why screening is essential to detect the condition.
However, some women may experience increased thirst, frequent urination, fatigue, or blurred vision, which are symptoms commonly associated with diabetes. Managing gestational diabetes is crucial to prevent complications for both the mother and the baby. If left uncontrolled, it can lead to various health risks, including:
What causes Gestational Diabetes?

Here’s a breakdown of the key factors contributing to the development of gestational diabetes:
- Hormonal Changes
- Insulin Resistance
- Genetic Predisposition
- Pre-pregnancy Health and Weight
- Age
- Previous History of Gestational Diabetes
- Ethnicity
Signs of Gestational Diabetes:
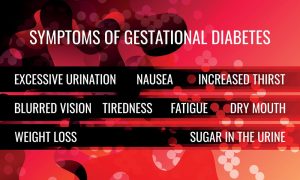
Here are some potential signs of gestational diabetes:
- Increased Thirst (Polydipsia): You may feel unusually thirsty and find yourself drinking more water than usual.
- Frequent Urination (Polyuria): Gestational diabetes can lead to increased urine production, causing you to visit the bathroom more frequently.
- Fatigue: Feeling fatigued, even after adequate rest, can be a sign of gestational diabetes.
- Blurred Vision: Some women may experience temporary vision changes, such as blurred vision.
- Increased Hunger (Polyphagia): You might find yourself feeling hungry more often or experiencing intense cravings.
It’s important to note that these symptoms can also be typical of pregnancy or other conditions, so they are not definitive indicators of gestational diabetes. Routine prenatal screenings, including glucose tolerance tests, are essential for diagnosing gestational diabetes accurately.
How is Gestational Diabetes Diagnosed?

Here’s an overview of the two common tests used for diagnosing gestational diabetes:
Glucose Challenge Test (GCT):
The glucose challenge test is a preliminary screening test used to identify women who may have a higher risk of gestational diabetes.
Glucose Tolerance Test (GTT):
The glucose tolerance test is the definitive test used to diagnose gestational diabetes. It is conducted after an abnormal GCT result or in cases where there are risk factors for gestational diabetes.
The diagnostic criteria for gestational diabetes can vary slightly depending on the guidelines used by different healthcare institutions, but generally, if you have at least two elevated blood sugar values during the GTT, you will be diagnosed with gestational diabetes.
If you are diagnosed with gestational diabetes, your healthcare provider will work with you to create a management plan to keep your blood sugar levels under control throughout the rest of your pregnancy.
How to treat Gestational Diabetes?

Here are the main components of treating gestational diabetes:
Medical Supervision:
Regular prenatal check-ups are essential for monitoring pregnancy and managing gestational diabetes. Your healthcare provider will closely monitor your blood sugar levels, assess the baby’s growth and development, and provide guidance on managing the condition.
Healthy Diet:
Following a balanced and nutritious diet is crucial for managing gestational diabetes. Work with a registered dietitian or a healthcare provider to create a personalized meal plan that includes the right mix of carbohydrates, proteins, and fats. The goal is to stabilize blood sugar levels while providing essential nutrients for both you and the baby.
Physical Activity:
Regular physical activity can help improve insulin sensitivity and regulate blood sugar levels. Engage in safe and moderate exercises recommended by your healthcare provider, such as walking, swimming, or prenatal yoga. Avoid prolonged periods of inactivity, as it can negatively impact blood sugar control.
Blood Sugar Monitoring:
Frequent monitoring of blood sugar levels is vital to understand how your body responds to diet, exercise, and other treatments. Your healthcare provider will guide you on how often to check your blood sugar levels and what target ranges to aim for.
Medication or Insulin Therapy:
In some cases, lifestyle changes alone may not be sufficient to control blood sugar levels adequately. Your healthcare provider may prescribe oral medications or insulin injections to help manage gestational diabetes. These medications are generally safe for use during pregnancy and are essential for maintaining stable blood sugar levels.
Self-Care and Education:
Educate yourself about gestational diabetes, its management, and potential complications. Learn how to administer insulin (if prescribed) and take proper care of yourself during pregnancy. Following your healthcare provider’s instructions and attending any educational sessions or support groups can make a significant difference in managing the condition.
Regular Foetal Monitoring:
Your healthcare provider may recommend regular fetal monitoring to ensure the baby’s well-being. This can include ultrasounds to check the baby’s growth and non-stress tests to assess the baby’s heart rate.
Closely Follow Healthcare Provider’s Recommendations:
It’s essential to follow your healthcare provider’s advice diligently and attend all recommended prenatal appointments. They will adjust your treatment plan based on your individual needs and how your body responds to interventions.
How to prevent Gestational Diabetes?

Maintain a Balanced Diet:
Eating a well-balanced diet is crucial for preventing gestational diabetes. Ensure you eat a range of nutrient-dense foods, such as whole grains, lean proteins, fruits, vegetables, and healthy fats. Steer clear of processed foods, sweet treats, and consuming too much-refined carbohydrates. Portion control is essential, as overeating can lead to weight gain, which is a risk factor for gestational diabetes.
Exercise Regularly:
Staying physically active during pregnancy is beneficial for both the mother and the baby. Engage in low-impact exercises like walking, swimming, or prenatal yoga. Regular exercise can help control weight gain, improve insulin sensitivity, and reduce the risk of gestational diabetes.
Monitor Weight Gain:
Keep track of your weight gain during pregnancy. Gaining weight at a healthy rate is essential, as excessive weight gain can increase the likelihood of gestational diabetes. Work closely with your healthcare provider to set appropriate weight gain goals based on your pre-pregnancy weight and overall health.
Stay Hydrated:
Proper hydration is essential for a healthy pregnancy. Drinking plenty of water can help regulate blood sugar levels and support overall well-being. Avoid sugary beverages and opt for water, herbal teas, or naturally flavored water instead.
Limit Caffeine Intake:
While moderate caffeine consumption is generally considered safe during pregnancy, excessive intake may be linked to an increased risk of gestational diabetes. Limit your daily caffeine intake to a moderate level or switch to decaffeinated options when possible.
Manage Stress:
Stress can have adverse effects on blood sugar levels. Implement stress-reduction techniques such as meditation, deep breathing exercises, or prenatal yoga to promote relaxation and emotional well-being.
Get Enough Sleep:
Proper sleep is vital for a healthy pregnancy and can help regulate hormones and blood sugar levels. Aim for 7-9 hours of sleep per night, and establish a regular sleep routine to improve sleep quality.
Regular Prenatal Check-ups:
Attend all scheduled prenatal appointments and discuss your concerns with your healthcare provider. Regular check-ups allow your doctor to monitor your health, provide guidance, and detect any potential issues early on.
Know Your Family History:
If you have a family history of diabetes, share this information with your healthcare provider. Being aware of your genetic predispositions can help your doctor tailor a personalized prevention plan.
Follow Medical Advice:
If your healthcare provider identifies any risk factors or potential warning signs of gestational diabetes, follow their advice diligently. They may recommend additional screenings or specialized care to manage your condition effectively.
Buy Gestational Diabetes Medicine:

Gestational diabetes can have potential risks for both the mother and the baby if not managed properly. Elevated blood sugar levels during pregnancy can lead to complications such as macrosomia (large birth weight), premature birth, and respiratory distress syndrome in the baby.
While insulin is the most commonly used medication for gestational diabetes, there are no specific oral medications approved for this condition. Many oral hypoglycemic medications are not recommended during pregnancy due to concerns about their safety for the developing baby.
As a result, insulin remains the gold standard for medical treatment in cases where lifestyle changes alone are insufficient. A few of the medicines are Glumetza, Glucophage, Metformin, Glynase, Diabeta, or Micronase (Glyburide). One can buy online gestational diabetes medicines from OffshoreCheapMeds at a fairly good rate.
FAQs:
What happens if gestational diabetes is not controlled?
It can lead to high sugar in the baby and the mother risking both permanent diabetic conditions.
Does gestational diabetes go away?
The majority of women with gestational diabetes experience a quick recovery after giving birth. Type 2 diabetes is a form of diabetes that does not go away. Even if the diabetes does go away after the baby is born, type 2 diabetes subsequently develops in half of all women who had gestational diabetes.
How do you get gestational diabetes?
Gestational Diabetes occurs in pregnant women who are unable to produce adequate insulin in the latter stages of their pregnancies.
Is gestational diabetes genetic?
Yes, it can be inherited from the parent body. A number of unidentified genetic, physiological, and environmental variables bring on this condition.
How common is gestational diabetes?
16.7% of the 21.1 million live births in 2021, or around 21.1 million, were affected by hyperglycemia in some way. In low- and middle-income nations with restricted access to maternity care, the syndrome is more prevalent. Henceforth, this kind is common and we should be aware of how to prevent gestational diabetes.

